Recently, a new study conducted by researchers at the University of Cambridge in the United Kingdom looks at the role of inflammation in the brain and its contribution to the development of different types of dementias.
More precisely, the researchers assessed participants with a diagnosis of any form of frontotemporal dementia, which is a type of dementia that primarily affects the frontal or temporal lobes.
A person with frontotemporal dementia is likely to experience a severe decline in cognitive abilities. The location plays a fundamental role in determining the impact of dementia. The effects can range from memory loss to difficulties in speech as well as personality changes.
The age-group that is most vulnerable to developing any kind of dementia in adults over the age of sixty. Some people may also develop early-onset dementia in their early thirties especially if they have a genetic disposition.
In addition to genetic disposition, a number of other factors play a role when it comes to the development of dementia including diet, lifestyle, medical history, environmental factors including exposure to toxins, and even social life.
RELATED: Breakthrough Research Identifies A Potential Treatment For Ulcerative Colitis
However, the exact cause and mechanism behind the development of the health condition have not been identified yet. Health experts suggest that the disease is multi-factorial and there may not be a single and leading cause for it.
Currently, there are is no available cure for dementia. Appropriate medical attention can only help in managing symptoms that can stop further degeneration of the brain and loss of cognitive abilities.
The new research, whose findings appear in Brain: A Journal of Neurology, looked at the role of neuroinflammation and its primary role as a contributor in frontotemporal dementia. The researchers also stated that the findings may apply to other neurodegenerative diseases in addition to dementia.
In order to reach this conclusion, the researchers looked at thirty-one participants with different types of frontotemporal dementia. Ten of these participants had the nonfluent variant, eleven had the semantic variant, and ten had the behavioral variant.
Previous research has associated the release of proteins including tau and TDP-43 to accumulate in the brain, causing disruption in the normal brain functioning and hence leading to dementia.
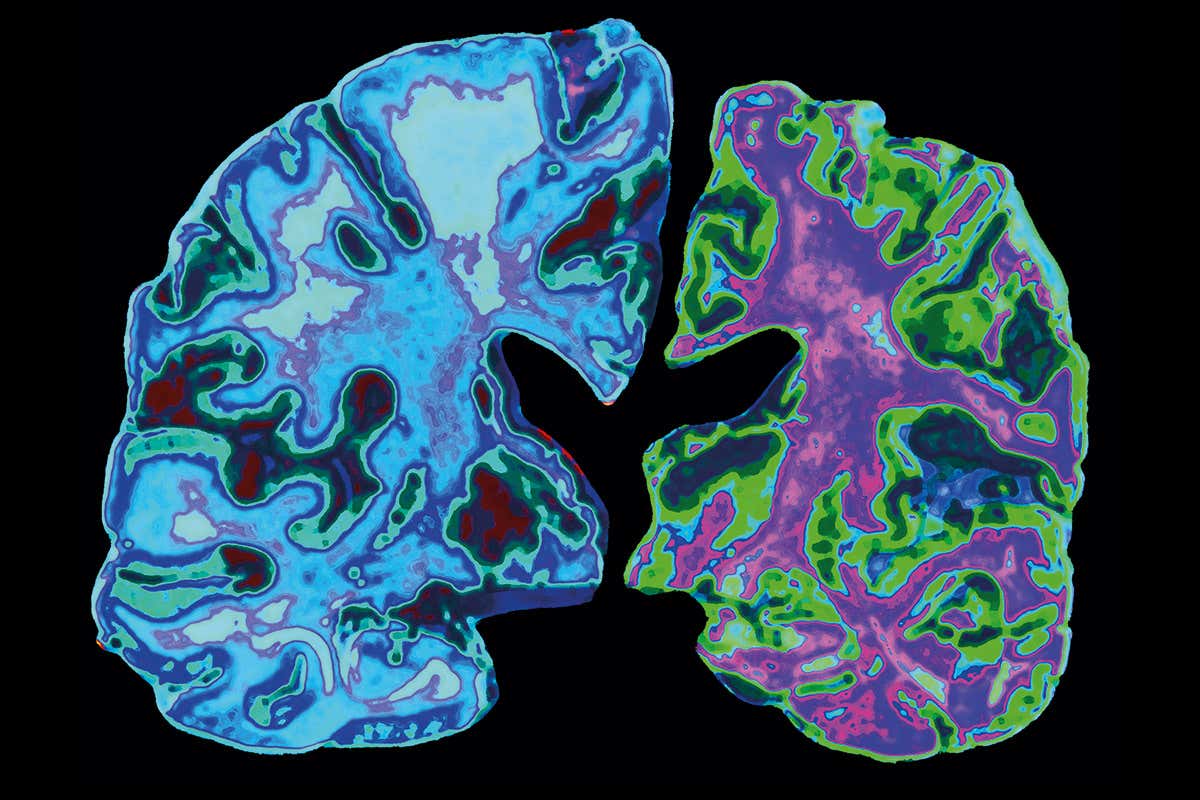
The researchers were interested in seeing whether inflammation can aggravate or has an association with the release of these proteins. To do so, they looked at PET scans of the brains of the participants which allowed them to identify any inflammation markers.
In the brain scans, it was noted that all of the participants with different types of frontotemporal dementia had an increase in inflammation markers. This further caused an increase in the release of tau and TDP-43 proteins.
These findings were also later confirmed via post-mortem of twelve brain donors who had donated to the Cambridge Brain Bank.
Dr. Thomas Cope, who is the co-author of the study, states “We predicted the link between inflammation in the brain and the buildup of damaging proteins, but even we were surprised by how tightly these two problems mapped onto each other,”
In addition, the researchers also stated the possibility of the procedure being circular which means that both inflammation and proteins trigger each other and cause neurodegeneration of the brain.
These findings are important not only for dementia but also in understanding different neurodegenerative diseases of the brain in general. Further research can help in a potential new treatment for dementia.