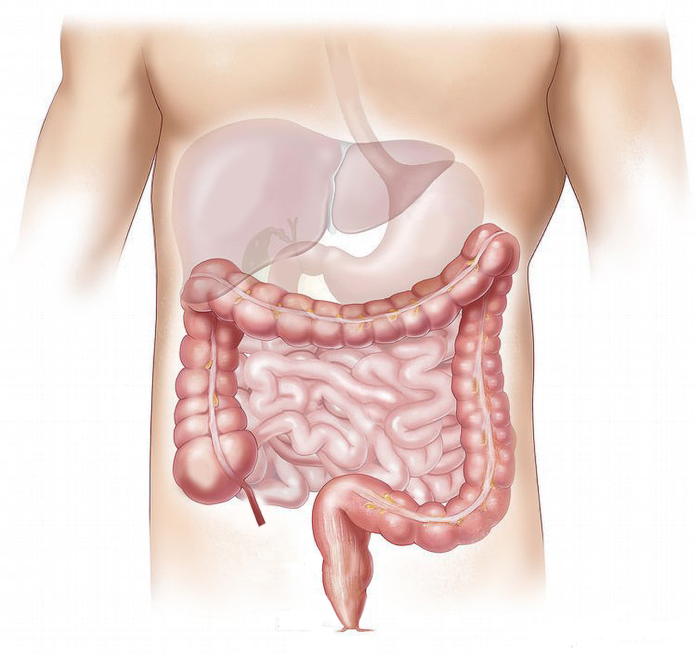
Doctors are mystified with the fact that small intestine cancer is highly unlikely but colorectal cancer which affects only a small organ actually accounts for the highest cancer-related deaths in the world. Is there something that researchers are missing while studying colorectal cancer development?
Yinon Ben-Neriah and Dr. Eliran Kadosh, from the Lautenberg Center for Immunology and Cancer Research at Hebrew University of Jerusalem (HU), ‘s tried to find this link studying the cancer mutations. They found that these mutations are not always bad actors to initiate colorectal cancer development. In fact, sometimes these mutations actually safeguard the body from cancer.
Also read- Dry Eyes Disease is Highly Common During Coronavirus Pandemic
Considering the metabolites produced by the human gut, antioxidants that are naturally found in black tea, berries, and hot chocolate are more likely to increase these metabolites. It means taking a high amount of black tea, berries or chocolate may aid in providing a favorable environment for the development of colorectal cancer.
The complete study findings are published in the journal Nature.
This research team tried to take a closer look at the gut cancers, trying to understand why small intestine cancers are only 2% and colorectal cancer development accounts for 98% cancers in humans.
One key factor between these two organs in gut microflora. The microbes in the small intestine are limited but in the colon, there is no end to their number and types. Researchers have emphasized on gut microflora associating it with overall good health and immunity. But its role in colorectal cancer development is relatively less familiar.
A common cellular gene TP53 produces a protein which is named p52. This protein works as a barrier to the cell and often plays a role in suppressing any genetic mutation to be taking place in cells. But when this protein is damaged, it doesn’t play its role in cellular protection. So the mutations result in cancers to grow rapidly and affect all parts of the body.
To verify the role of gut microflora in colon cancer development, the research team added a mutated version of the p53 gene in the gut. The small intestine changed this mutation and converted it back to the normal, effectively playing its role. But the same mutated gene in the colon didn’t experience any such thing. In fact, it promoted the spread and growth of cancer.
This outcome is sufficient to determine the role of gut microflora in the development, growth, and spread of cancer. To test this theory more, the research team introduced antibiotics to ward off the gut microflora. Once these microbes were killed, there was no change to the p53 function in spreading cancer, on its own.
Also read- Hepatitis C Infection is Now Treatable
The gut microbes produce metabolites which are also called antioxidants. When a person takes foods that are rich in the same antioxidants it increased the inner load and the efficiency of p53 protein is compromised. This is more likely to affect people with a family history of colorectal cancer.
These findings suggest that these people should pay attention to what they feed to their bodies. Those with a direct and clear family history should acknowledge it and change their dietary preferences accordingly.